Bedford Hospital
(South Wing)
1965–1971

Photograph: Authors collection
Josie and I left Goldington Road Bedford in 1965 and moved to Sexton Avenue in Kempston. Mr. Smith moved into a nursing home this home was just a few doors from where he lived and owned by his daughter in law. I obtained two further employments but neither position was suitable for me, Josie pointed out an advert in the local newspaper for General Porters at Bedford Hospital, (South Wing). I applied and was interviewed by a Mrs. Small the hospital secretary, and the head porter a Mr. Reg. Heart, I was successful and started work the following week.
The shifts were alternating round the clock, 0600-1400 then 1400-2200 and 2200–0600 with 0900–1700 as required. It was mainly routine work but interesting and varied, one job was going to the operating theatre to fetch patients and return them to the wards; it was during one of these trips a Sister H approached me. She was the senior sister in the operating theatres, whilst I was waiting for the patient to come out of the theatre she asked, “would you consider working with us here as a theatre porter”? “Yes I would be pleased to,” I replied, without really thinking about the implications although in hindsight it was a good move.
A week later I was wheeling patients from the wards to theatre and returning them after their operations. I worked with a man named George Roberts a happy person and a good man to work with.
Patients were often worried and understandably so, not sure what was going to happen to them. The operating theatre was always a bit of a mystery and probably still is to most people.
Delivering patients to the theatre and returning them to the wards was for the most part quite straightforward. Russell, Arnold Whitchurch, and Gifford Nash wards were all on the first floor and accessible by stairs or lifts. The problems arose when the lifts broke down or had to be serviced. It was then the patients had to be carried downstairs, and back up after their operation. (We had no recovery room in those days.) From Gifford Nash ward there were 5 flights to negotiate and a total of 28 steps changing direction, and the same for other first floor wards. Sometimes a patient would try to hang on to the banister and that could turn into a dangerous situation. Or they would start to come round halfway up the stairs on the return journey, thankfully this did not happen very often.
A doctor Hosford was the senior consultant anesthetist I was responsible to him as well as Sister Hugett. Timing was always important with the doctors; they usually wanted the patient in the anesthetic room 15 minuets before the start of the operation. Several things I noted with Doctors generally, they hated being kept waiting but they never seemed concerned about keeping others waiting. When not fetching and returning patients to their respective wards, I was encouraged to work in the theatre and assist Doctor Hosford and his team of anesthetist’s by laying out their equipment and positioning the patient’s on the operating table as required.
About 8 months after I started work in the theatres George Roberts decided to change departments and move to the mortuary.
Dr. Hosford. and Sister Huggett asked me to take over Georg Roberts responsibilities in the theatre, I accepted. I would have to attend two courses in London for further training; one was held at Hillingdon Hospital and another at Edgware Hospital. Although they were short residential courses they were important, and full of good practical information, I was now classed as a theatre attendant. My duties were varied, and I was responsible to the anesthetist’s. The duties included: Washing cleaning the equipment when required. The walls and floors were cleaned once every day and as required, this was normally carried out during the lunch hour. Other duties included
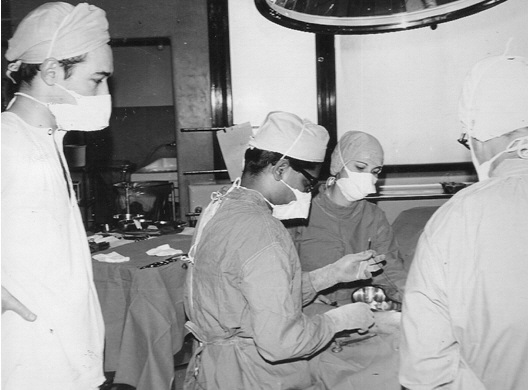
C 1967 in Theatre
L-R L. the Author, Dr. Sam, Staff Nurse J, Dr. P.
Setting up the anesthetist’s trolleys with drugs and equipment, making sure the gas bottles were in good order and full, changing them when necessary. Sterilizing the laryngoscope blades, airways, forceps, and other equipment that may be required. Assist with intubation and passing the right equipment at the right time, positioning the patient if an epidural nerve block was required; ensure the lighting was correctly positioned. Take samples of tissue to the pathology department and collect blood when required. And make sure we had the correct cross matched blood for the correct patient.
Counting the swabs before and after the operation, recording the numbers in units of five. Ensuring the right theatre furniture was assembled at the right time. For example, if lithomitey poles were required, provide them, and make sure the anesthetized patients legs were lifted into position with care and both together. If the diamerathy unit was in use, place the pad on the limb in the correct position. It was often my duty to watch over the patient if the anesthetists had to go through to the twin theatre for any reason. The theatres were designed so that we were in each others view all the time. If amputation took place discreetly dispose of the limb. Fetch blood from the pathology department Orthopedic days were normally Tuesdays, many bloodless operations took place; these were lower and upper limb operations, either from the knee downwards including the feet and toes, or from elbow downwards and including the hands and fingers.
This was achieved by first raising the limb, then using a rubberized (Esmarch) bandage and applying it tightly from the toes or fingers to above the knee or the elbow, then using a tourniquet to stop the blood flow.
It was important that I always recorded the time of application and reminded the operating surgeon the length of time it had been applied.
As well as general abdominal and orthopedic surgery, there were ophthalmic, dental, and what I termed as a cystoscopy session and minor operations period which was in the main the removal of lumps and bumps, then often the emergency operations which could happen at any time.
Emergency operations that I remember were, appendectomy (removal of the appendix), these patients were often in considerable pain, removal of the spleen because of major blood loss, this happened when the spleen was ruptured, usually due to a to a serious road accident. Very serious cases often had to be brought to the theatre on their bed, anaesthetized, and then transferred to the operating table.
Working in the theatre we normally finished at about 1800, however one more special job had to be performed. That was the preoperative shaving for the operations that were to be preformed the next day. Anywhere on the body an operation was to take place had to be free of hair, this meant a clean close shave. One patient I remember well was a retired local Police Sergeant I will call him Sergeant K. He was well known locally, I reassured him I had not come to shave off his large ginger mustache, and jokingly said that quite a few criminals would like to be in my position just now. For the most part this shaving procedure was quite straightforward, except if the patient was very shy or nervous.
Earlier I mentioned some doctors hated being kept waiting. On several occasions I would be in the middle of the shaving when a doctor arrived to examine the patient. I would be asked to leave so that the doctor was not delayed.
This usually meant leaving the patient wet with soap and sometimes half shaven around the pubic area. Later I would be called back to complete the job. I always considered this bad practice and bad manners by the doctors concerned. Another annoying thing was how some nurses did what I term as sucking up to the senior doctors. Yet the same nurses could be quite offhand to the junior doctors and other staff, including me. That was unless they wanted something such as an errand, “would you be a love, nip out and
get me some cigarettes?” It was then they could be quite charming, that said, they were all contentious and hardworking and very dedicated to their profession. And for me it was an interesting and rewarding job, because I was learning by practical experience rather than study. I enjoyed my time in the theatres however the pay was poor, and shift work within the hospital would be better.
 One very interesting part of the job was to take photographs when necessary, usually of specimens that had been removed. They were used for training student nurses or for use in the medical institute. Mr. P a consultant surgeon often asked me to use his camera, at other times I used the hospital camera, but for the most part I used my own which was much more reliable. Mr. J W. requested me to photograph several of his patients; at one time I had quite a large collection of medical photographs taken with my camera and film most of which I gave to various doctors when I left the Hospital.
One very interesting part of the job was to take photographs when necessary, usually of specimens that had been removed. They were used for training student nurses or for use in the medical institute. Mr. P a consultant surgeon often asked me to use his camera, at other times I used the hospital camera, but for the most part I used my own which was much more reliable. Mr. J W. requested me to photograph several of his patients; at one time I had quite a large collection of medical photographs taken with my camera and film most of which I gave to various doctors when I left the Hospital.
The most interesting set of photographs of an operation that I was involved with during my time working in theaters happened to take place on a Sunday afternoon. It was a regular requirement for me to call into the hospital at 1500 to visit the wards and perform the shaving requirements for the Monday operations. As I picked up the list from the theaters emergency teams were gathering and preparations were being made for the arrival of the patient.
I enquired, “What’s the emergency today, staff nurse? – Oh Mick, we may need you, we have a male patient with a aortic aneurysm on his way down, Mr. Hadfield will be starting the operation as soon as he arrives”. I set off for the wards and soon had my job done, there were just four shaves to complete and I was back in theaters within half an hour; the patient had arrived and Mr. Hadfield and the team were scrubbing up. I had not heard of this condition before, therefore I was most interested.
Aortic dissection is a tear in the wall of the aorta that causes blood to flow between the layers of the wall of the aorta and force the layers apart. Aortic dissection is a medical emergency and can quickly lead to death, even with optimal treatment. If the dissection tears the aorta completely open (through all three layers), massive and rapid blood loss occurs. Aortic dissections resulting in rupture have an 80% mortality rate, and 50% of patients die before they even reach the hospital. If the dissection reaches 6 cm, the patient must be taken for emergency surgery.
It was not long before Mr. Hadfield started the operation and I helped as helper / runner for a doctor B Bazley who was the anesthetist; it was an interesting protracted major operating procedure, it required a Teflon replacement of that part of the aorta. From memory I believe this operation took about 5 hours. Sadly the man concerned died the day after the operation had been completed.
Casualty
Times were changing in my life and family; we now had two children. It was early in 1968 and I decided to return to shift work as a casualty porter. This would enable me to earn a little more money. As it turned out it was just as interesting as working in the operating theatre and sometimes more so. It was around the clock shift work including weekends. We had the usual routine jobs which had to be carried out for the most part it was the transport of patients to the many departments and wards around the hospital estate. Helping to undress severely injured people was often a very difficult procedure, and especially so if they were overweight or semi conscious. Sometimes patients had consumed too much alcohol and were in a fighting mood.
We had a young man come into casualty one Saturday evening having sustained an injury at a rugby match during a game in the afternoon. After the match he decided to go for a drink (as they do) and woke up in the casualty department just as I was trying to undress him. As I later learned, he thought I was responsible for his pain. I could see what was coming, (he may just as well have sent a postcard.) He took a swing at me, I ducked, he missed, and he fell off the trolley, hurting himself a bit more.
However nights and weekends were so much more interesting we had to deal with all sorts of different situations, ranging from dog bites to stabbings. Fatal accidents that came through casualty at night time or weekends we delivered to the mortuary. I escorted relatives to view the body. Sometimes the Coroner’s Officer P.K. was in attendance for identification of the body. On occasions it was a difficult and often distressing job.
The Two Story’s below concern both the Fire Service and the Hospital
Fire Control Britannia Road Bedford 2nd April 1969.
At this time I still worked at the Hospital but was involved with the Fire service a well.
The fire control nightshift came on duty at 1800; at 1831 a message was received from the police concerning children buried in a sandpit near Shefford close to the A600. At 1833 Shefford fire station mobilized with a water tender and land rover with leading fireman Brown in charge. They arrived at the scene just 3 minutes later. At 1835 the deputy chief fire officer and chief fire officer were both informed. D.C.F.O Ron Drought proceeded to the incident. At 1846 Leading Fireman Brown sent an informative message that three children had been dug from under the sand.
The firemen used their hands to drag the sand away. A further search was in progress to eliminate the possibility of other children buried. At 1903 D.C.F.O. Drought sent a message that three children had been removed to hospital by ambulance.
The Stop message was sent at 1956. On that Wednesday 2nd April 1969, I was on duty in the casualty department working the afternoon shift 1400–2200. At around 1900 the sister on duty called me to one side.
“Mick, we have some children coming in by ambulance we do not expect them to come in to casualty, when they arrive would you go and open the mortuary”?
Not many minutes passed and the Ambulance reversed into the parking bay, a doctor and nurse entered, after examination they re-emerged. I made my way to the mortuary which was situated close by.
We carried the three children from the ambulance and with care placed them in the cool container. Some time later in the evening Police Sergeant P. K. the coroner’s officer arrived with a relative of two of the children, this was for the identification procedure. This was a sad and tragic event. The children were John Pierce age nine, his sister Gillian age four, and Martin Ridgway age seven.
The Coroners inquest was held in Bedford and reported in the Bedfordshire Times on the 2nd May 1969. Doctor Max Lucas returned a verdict of death by misadventure on the three children concerned. Doctor Lucas also stated that death was due to asphyxia, and there is no evidence of criminal negligence.
Collie Road Bedford
17th January 1969
The emergency 999 call was received at Britannia Road Fire Control at 1422 the caller stated: “Fire in bedroom” and then hung up, fortunately the call was traced to 27 Collie Road Bedford. The water tender from Bedford station booked mobile at 1424 and were in attendance at 1428 with Station Officer Hull. At 1430 Leading Fireman Lazenby sent a radio message to control, “bedroom well alight” then at 1432 another message was sent from Station Officer Hull, “ambulance required persons trapped.” Mr. Edwin Green age 39 was in bed and it was on fire, due to being part paralyzed he was unable to reach the bedroom door of his house or his wheelchair, but was able to dial 999 from his bedside telephone. The Fire service broke into the house; rescued Mr. Green with his bedding and pajamas on fire which the firemen soon extinguished.

The Humber Rescue Unit 1969. Photo Author
At 1435 a request was made for a minuteman oxygen resuscitator and the rescue unit was ordered on. At 1439 an informative message was sent by Station Officer Hull, “One male person rescued, urgently awaiting ambulance”.
The Stop message was sent at 1451 and Mr. Green arrived at casualty by ambulance at about the same time. I received the patient and helped remove what was left of his burnt bed clothes. He had been brought into casualty on a Fire Service salvage sheet. Mr. Green’s burns were severe both to his lower limbs and his right arm; after the burns were cleaned and the patents condition was stabilized he was transferred to Mount Vernon Hospital, I did not hear the final outcome or weather Mr. Green survived the serious burns he suffered. It was at 1600 a fireman called to retrieve the salvage sheet, and that was the first time I met Charles Mattin.
August 1969
ne Wednesday evening the Fire Brigade came into the hospital casualty car park, it was almost empty. The Chief Fire Officer (C.F.O.) Norman Richards had arranged an evening to demonstrate the equipment the fire engines carried to the staff at the hospital. This was for those that were interested and wished to attend; I was in the front row and found it very interesting.
During the course of the evening C.F.O. Richards chatted to everybody, including me he explained that the men on duty that evening were a mixture of whole time professionals, and part time paid volunteers.
My mind was thinking, perhaps I could join up and work for the Fire Service in my off duty hours, this would boost my income and it would be an interesting worthwhile enterprise. I had a few skills such as casualty handling, first aid, and knowledge of trauma and shock. Within a few weeks I had been to an interview at Britannia Road H.Q. and was accepted as a retained fireman, a good news day, and a new pathway.
My main employment was still at Bedford Hospital but when off duty I would be on call for Bedfordshire Fire Service
Carbon Monoxide Poisoning
Tuesday 16th December 1970.
Bedford.
At this time I was working for the hospital as porter in casualty also as a retained (part time) Fireman.
This in my opinion was one of the most tragic cases I witnessed whilst working in the casualty department at Bedford Hospital; it was the death of seven people, five from one family and two from another. From memory it was around lunchtime that a staff nurse informed me, “Mick we are going to be busy in a few minutes.” Often the casualty department was warned by radio or telephone when to expect several casualties at one time. A few minutes later two ambulances arrived at the entrance, followed a little later by a third. Three young children were laid on trolleys I had prepared, the two youngest were placed one at each end of one trolley and a third on another, they were held to one side whilst other members of the family were taken into the two main resuscitation rooms. A doctor examined the three children, almost immediately and in my own mind I knew they were dead. There were a total of eleven casualties from this one house, seven were dead and four survived. I helped where and whenever possible, Sergeant Peter K called in briefly during the afternoon and visited the mortuary.
The two families involved lived in a large shared house at, 44 Polhill Avenue Bedford Mr. Nicholas Sasko age 51 a greengrocer, his wife Joanna aged 42, their three children Marino aged 9, Wendy aged 7, and Christopher aged 3. Mrs. Anna Di Iulio aged 21, and her baby Giacomo just 6 months old. Four other people Lugigi Di Iulio Anna’s husband; Costa Sasko 15; Natasha Sasko 13 and Aristotle Sasko were found unconscious and taken to hospital
where they recovered.
The Coroners Officer Sergeant Peter K said that death was due to carbon monoxide poisoning and this had been confirmed by analysis, all seven bodies had been identified on the afternoon of December the 16th by a relative. There were rumors and speculation in the Bedfordshire community as to what was going on in the household at 44 Polhill Avenue at the time of this tragic accident.
Statement
A statement from the assistant chief constable Mr. Anthony Armstrong was read at the inquest by Mr. Keith Rose representing the Sasko family.
“In the course of our investigations into the death of Mr. And Mrs. Nicholas Sasko and three members of their family, we discovered no evidence of criminal activity by the late Mr. Sasko. There was nothing in the house that indicated trafficking in stolen goods or the production of illicit alcohol. In the interest of surviving members of this family the police feel the above should be made known.
A Mrs. Olszanski (family friend) wrote a letter to the Coroner Dr. Max Lucas on January 12th, the letter was read out before the inquest began.
Mrs. Olszanski told how; she received a telephone call from Mr. Costa Sasko on the Monday saying that everyone in the house was ill. The family doctor had called to see them and said that they were all suffering from flue. He apparently told Costa they were in no danger. Mrs. Olszanski made another telephone call to the house the next day and got no reply, she then phoned their family doctor herself to request a further visit but was informed that they were suffering from flue. Later she visited the house herself and the tragedy was discovered. At the conclusion of her letter Mrs. Olszanski wrote: “I wish to say that, in my opinion the diagnosis of the illness was not a proper one in the circumstances. The fact that a second visit by the doctor was not made may have been a contributory cause of death.”
In his summing up, Dr. Lucas cleared the doctor of any negligence. He said: “As far as I can see it was in the minds of the doctor and his patients that they were suffering from a natural illness and this required nursing at home in bed.”
“I cannot think for a moment of anything to suggest that any other factor, like carbon- monoxide poisoning could have presented its self to his mind, I can find no evidence of negligence. They were all given medicine for a natural illness and time was allowed to see what the effect of this treatment would be”.
The Cause
A seven man jury was informed that cotton sheet had been draped over the front of a gas central heating unit which required good ventilation. A warning notice on the on the heating unit read: “Warning —- articles must not be stored near to, or touching, the air heater, water heater or flue. Nor must they block any grill in the heater surrounding the structure.” The jury was informed that Mrs. Sasko could not read English and she did not speak it very well.
One Night in Casualty
It is worth mentioning at this point there was often a shortage of staff at night time and at weekends. On night duty there was just one staff nurse and porter, plus a doctor on call. I am of the opinion that we, the porters, often provided services that was far beyond anything we were trained to do or paid. But we just got on with a job that had to be done. I am of course writing this in hindsight, but I believe the hospital authorities took advantage of us and what we were willing to do.
Night duty was from 22.00 until 06.00 the next morning. The busy nights were usually Fridays and Saturdays, however things could change very quickly even in the small hours of a weekday.
On night duty the porter often had to make decisions, and act on them if he felt it was necessary, for instance if the Staff Nurse was busy. Over the years I have thought long and hard as to whether I should relate this story, but I think now it is time to tell. It was midweek at about 23.00. The duty staff nurse that evening was not the regular nurse I worked with and I will give her the name as Nurse B.
Our regular night staff nurse was a gem and good to work with I will call her, nurse O. Unfortunately she was on holiday the night in question.
Suddenly a man came through the casualty doors walking and clutching his face, he was hemorrhaging severely. As I got him onto the trolley to take him into the examination room his hand moved slightly away, I could see he had a deep wound that ran from the top of his forehead to the base of his chin. His face in part was hanging open, he told us he had been in a fight, and he had an American accent.
Nurse B started to undress him for examination by the doctor; I cleaned up the blood on the floor. Just as I was finishing the cleaning, another man came walking into casualty. He appeared to have a little bruising but nothing serious, nurse B was busy dealing with the first patient. I took the second man to a cubical to sit down and take his details. This man had also been in some sort of fight, he was acting in a rather odd manner often looking up and down the corridor, and I suddenly realized this was probably the person that had caused a terrible injury to the first man.
At this time Nurse B and the Doctor were busy treating the first man and I was becoming concerned and I decided to inform the police, this I did from a small room nearby. As I finished the call, a police constable I knew well walked into casualty I will call him X. He was a dog handler and his dogs name was Amos, “wow that was quick X it did not take you long”. “What’s up Mick”? He enquired, I quickly explained the situation and where the men were situated, police control were calling him on his radio; he called back to say he was already at the hospital. Actually, he had been passing the entrance and decided to call in for a cup of tea, which was the norm in the late 1960s.
He walked quietly up and down the corridor with his dog Amos; I was standing in the corridor a few feet away from the patient. A little later X went out and put his dog in the van, then returned to the cubical. The man concerned had not yet been seen by the doctor, about 15 minuets later when X was sat outside the room we conversed, he had arrested the man and recovered the bloodstained weapon that had inflicted the wounds. As soon as the doctor had seen this man he was taken into police custody and I later learned he was charged with grievous bodily harm, the first man who was severely injured was admitted to the wards.
Sometime later that evening Nurse B called me to one side; she gave me a severe reprimand for informing the Police telling me. “It’s not your job to phone the police,” and something about patient confidentiality, inwardly I was flabbergasted as I considered if there was a danger to staff or patients it was the best course of action, and in this case I really believed I was right, but to maintain good relations I did not argue and told her I was sorry.
Recently (2006) I was admitted to a large casualty department with a heart problem, just inside the waiting room was a permanent police office with two policemen checking up on who was coming in. I wonder how Nurse B would have dealt with the situation today. I gather Nurse B did well in her career and went on to higher things and I wish her well.